AI helps predict response to immunotherapy in lung cancer with real-world data from medical history and blood counts.

121 / 5.000
AI helps predict response to immunotherapy in lung cancer with real-world data from medical history and blood counts.
Research teams from the Universidad Politécnica de Madrid, CIBER, the Jiménez Díaz Foundation Health Research Institute, the University of Navarra Clinic, and the 12 de Octubre University Hospital have developed and validated an artificial intelligence algorithm capable of accurately predicting which patients will respond to immunotherapy based on real-world data (RWD).
The results of the study, published in Cancer Immunology, Immunotherapy, demonstrate that reliable predictions can be made using readily available information. This represents a further step towards personalised medicine, helping to improve treatment efficacy, focus clinical trials on patients at higher risk of disease progression, and minimise the occurrence of unnecessary side effects, as well as contributing to the reduction of healthcare costs.
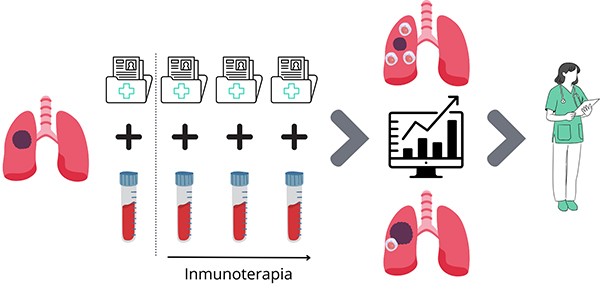
The study proposes a method to anticipate whether a patient with advanced non-small cell lung cancer will respond to immunotherapy. It analyses data from medical records and blood samples taken before and during the initial cycles of treatment. With the help of an artificial intelligence model, it is possible to accurately predict whether the tumour will progress, which is associated with greater activation of T cells and a more effective immune response against the cancer. This information could help physicians decide whether to continue or adjust the treatment in time.
María Jesús Ledesma, a researcher at the Universidad Politécnica de Madrid (UPM) and in the Bioengineering, Biomaterials and Nanomedicine area of CIBER (CIBER-BBN), explains that “the system is based solely on information available from the patient’s medical history and routine blood counts obtained during the first cycles of treatment, under the hypothesis that the response during the initial stages of therapy can provide clues about the patient’s long-term outcome.”
Lung cancer is the leading cause of cancer-related death worldwide, with a five-year survival rate of only 10% for the most advanced metastatic cases. In recent years, various therapies have been developed aimed at enhancing the immune response and blocking the mechanisms developed by tumour cells to evade it. These treatments are known as immunotherapies and have had a significant impact on the natural history of the disease and on treatment outcomes for patients. In addition to improved survival rates, immunotherapies are associated with a better quality of life, free from the widespread side effects typical of chemotherapy.
“Many studies have focused on deeply analysing the metabolic and cellular signalling pathways associated with the immune response. However, due to the variability in immune responses between patients, the effectiveness of immunotherapies is highly diverse, and a significant proportion of patients eligible for treatment still experience disease progression, even after initially appearing to respond,” explains Ana D. Ramos-Guerra, a researcher in Ledesma’s group at UPM/CIBER-BBN and first author of the article.
The authors explain that, to monitor the response, only data relating to the patient’s condition, immune-mediated adverse events, and routine blood tests performed during each immunotherapy cycle were used. “The proposed model uses information on the presence of metastases in the central nervous system, the onset of pneumonitis or colitis at the beginning of immunotherapy, and a diagnosis of type I diabetes, in addition to blood test variables such as lactate dehydrogenase levels, absolute lymphocyte count, and the platelet-to-lymphocyte ratio, all of which were collected over time.”
The work has been made possible thanks to the collaboration of teams from various institutions and hospitals. It was funded by the Ministry of Science and Innovation, through the State Research Agency, with co-financing from the European Regional Development Fund (ERDF). It has also received funding from the INGENIO project of the Carlos III Health Institute (ISCIII) and from the European Union’s Next Generation EU funds. Additionally, it was partially supported by a 2019 Leonardo Grant for Researchers and Cultural Creators from the BBVA Foundation and by the MAGERIT-CM project, within the R&D programme in Technologies of the Community of Madrid.
Bibliographic reference: Ramos-Guerra, A.D., Farina, B., Rubio Pérez, J. et al. Monitoring peripheral blood data supports the prediction of immunotherapy response in advanced non-small cell lung cancer based on real-world data. Cancer Immunol Immunother 74, 120 (2025).
https://doi.org/10.1007/s00262-025-03966-9
Source : `e-Politécnica Investigación e Innovación’ (nº 728), boletín de la UPM, published in its original source on 28 of April of 2025
Share this:
Latest news



Categories